Ketamine, originally developed as an anesthetic in the 1960s, has grown in its applications beyond the operating room to become a valuable tool in mental health and pain management. Known for its rapid-acting effects, ketamine works differently from typical medications by interacting with neurotransmitter pathways in the brain, providing unique benefits that are now being explored for both physical and mental health conditions. While initially controversial due to its potential for misuse as a recreational drug, ketamine has gained acceptance in the medical community when used in controlled settings, revealing its potential to help individuals manage severe depression, chronic pain, and even post-traumatic stress disorder (PTSD).
This article delves into what ketamine is, its history, how it functions in the body, its varied applications in modern medicine, and what potential benefits and risks it carries in the treatment of challenging health conditions.
1. Understanding Ketamine: History and Mechanism of Action
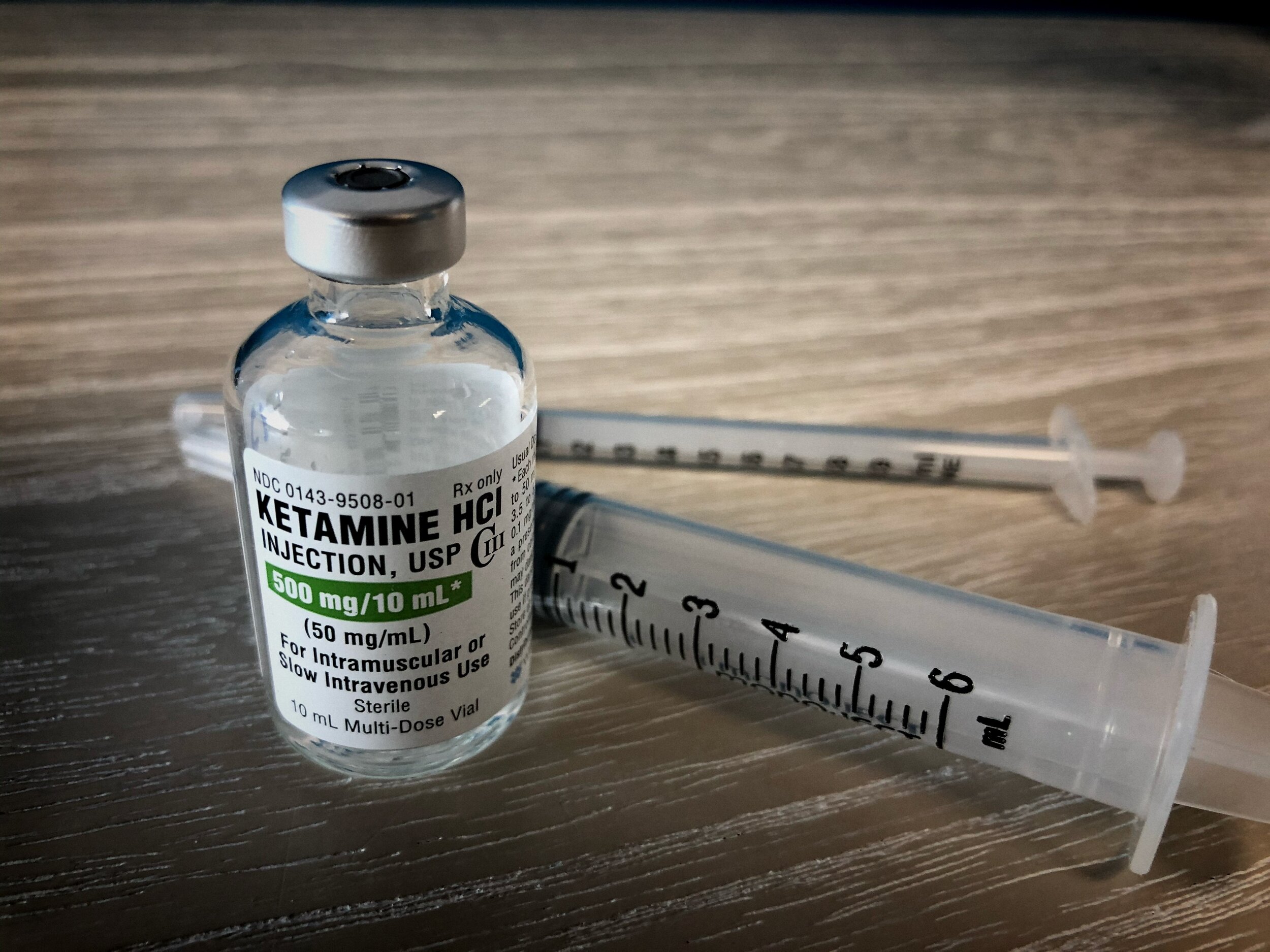
Ketamine, chemically known as ketamine hydrochloride, was first synthesized in the 1960s by American chemist Calvin L. Stevens as an alternative anesthetic with fewer side effects than phencyclidine (PCP), a drug notorious for its hallucinogenic effects. Approved by the U.S. Food and Drug Administration (FDA) in 1970, ketamine gained traction as an anesthetic primarily used in surgical and veterinary settings due to its ability to induce sedation without significantly depressing the respiratory system. Ketamine is classified as a dissociative anesthetic, meaning it causes individuals to feel detached from their bodies and surroundings while maintaining some level of consciousness, which is distinct from the unconsciousness induced by other anesthetics.
The mechanism of ketamine’s action is unique among anesthetics and mood-altering drugs. It primarily acts on the N-methyl-D-aspartate (NMDA) receptor, a part of the brain’s glutamate system. Glutamate is an excitatory neurotransmitter responsible for functions like memory, learning, and mood regulation. By blocking the NMDA receptor, ketamine disrupts the flow of glutamate, leading to changes in perception, mood, and pain sensation. This interruption in the glutamate system not only induces anesthesia but also affects the brain’s neural connections in a way that has been shown to have rapid antidepressant effects. Ketamine also has secondary effects on other neurotransmitters, including dopamine and serotonin, further contributing to its mood-altering properties.
The effects of ketamine are fast-acting, often taking effect within minutes when administered intravenously, and lasting from minutes to hours depending on the dose and individual. This rapid onset has sparked significant interest in using ketamine as a treatment for mental health conditions, as traditional antidepressants can take weeks to produce noticeable effects. Today, ketamine is used in a controlled medical environment to treat a range of conditions that are often resistant to standard therapies, though it remains a Schedule III controlled substance due to its potential for misuse and abuse.
2. Ketamine in Pain Management
One of the primary clinical applications of ketamine today is in pain management. Due to its ability to block NMDA receptors, ketamine can effectively treat chronic pain by disrupting the brain’s perception of pain signals, making it valuable for patients who suffer from conditions like fibromyalgia, complex regional pain syndrome (CRPS), and certain types of neuropathic pain. Unlike opioid painkillers, ketamine does not act directly on opioid receptors, reducing the risk of dependency. For patients who do not respond well to opioids or who have developed a tolerance, ketamine provides an alternative that can relieve pain without the high risk of addiction associated with opioid medications.
Ketamine is often used in low-dose infusions for pain management. These infusions allow for continuous administration over a specified period, providing relief that can last for days or even weeks after a single treatment. Chronic pain conditions are complex and often resistant to conventional painkillers, and ketamine infusions have been shown to help manage severe pain by modulating both peripheral and central nervous system responses. By acting on the NMDA receptors involved in central sensitization (a state where the nervous system becomes hypersensitive to pain), ketamine helps reduce the hypersensitivity to pain stimuli that is common in chronic pain conditions. Patients undergoing ketamine infusions for pain management often report immediate relief, followed by long-lasting reduction in pain severity.
In addition to chronic pain, ketamine is used in emergency medicine for acute pain relief in situations such as trauma or severe injury, particularly in military and combat settings. Because it does not depress respiratory function, ketamine is especially useful in situations where it may not be possible to closely monitor a patient’s breathing. Military personnel have used ketamine to manage pain in field settings, as it allows them to maintain consciousness and alertness while reducing the sensation of pain. This versatility makes ketamine an effective tool in both short-term and long-term pain management, adding a valuable option for patients who need an alternative to conventional analgesics.
3. Ketamine’s Role in Treating Depression and Mood Disorders
One of the most groundbreaking applications of ketamine has been in the treatment of major depressive disorder (MDD), particularly in cases that are resistant to standard antidepressants. Traditional antidepressants, such as SSRIs (selective serotonin reuptake inhibitors), typically require several weeks to become effective, and some patients may experience little to no relief even after prolonged use. Ketamine, by contrast, has shown rapid antidepressant effects in many patients, often reducing depressive symptoms within hours of administration. For those struggling with treatment-resistant depression (TRD), ketamine’s fast-acting properties can offer much-needed relief, especially for individuals who may be at high risk of suicide.
In recent years, ketamine has gained approval for use in specific forms of depression treatment. Esketamine, a derivative of ketamine, received FDA approval in 2019 as a nasal spray for treatment-resistant depression. The spray, administered in clinical settings, provides patients with a less invasive option that still benefits from ketamine’s antidepressant properties. Esketamine’s approval has marked a significant step in the use of ketamine for depression, making it accessible for those who may not tolerate or benefit from oral antidepressants.
Research into ketamine’s effects on depression has revealed that it not only impacts mood regulation but may also stimulate neurogenesis, or the growth of new neural connections in the brain. Depression is often associated with reduced neuroplasticity, particularly in areas of the brain involved in emotion and decision-making, like the prefrontal cortex. Ketamine’s ability to promote neural growth may help “rewire” the brain, providing lasting relief even after the immediate effects wear off. Patients receiving ketamine for depression typically undergo a series of infusions in a controlled clinical environment, with the number and frequency of infusions tailored to each individual’s response and needs.
4. Ketamine for Post-Traumatic Stress Disorder (PTSD) and Anxiety Disorders
Beyond depression, ketamine has shown promising effects in the treatment of post-traumatic stress disorder (PTSD) and certain anxiety disorders. PTSD, a condition resulting from traumatic experiences, often manifests as severe anxiety, flashbacks, and difficulty coping with stress. While psychotherapy and medications such as SSRIs are the first lines of treatment for PTSD, many patients find limited relief, leading researchers to explore ketamine as an alternative. Ketamine’s rapid onset and ability to alter brain pathways involved in stress response make it an effective option for patients who do not respond to traditional therapies.
The mechanism through which ketamine alleviates PTSD symptoms is similar to its effects in depression, with NMDA receptor blockade contributing to a reduction in hyperarousal and heightened stress response. In addition to blocking NMDA receptors, ketamine’s secondary effects on neurotransmitters such as serotonin and dopamine can help modulate mood, making patients feel calmer and less anxious. Ketamine therapy for PTSD is usually conducted under controlled medical supervision, often as part of a comprehensive treatment plan that includes psychotherapy. Some clinics also incorporate “ketamine-assisted psychotherapy,” where ketamine is administered before therapy sessions to enhance therapeutic outcomes by reducing the psychological barriers associated with traumatic memories.
Studies on ketamine’s effects on anxiety disorders, such as generalized anxiety disorder (GAD) and social anxiety disorder, are ongoing. While traditional anti-anxiety medications, like benzodiazepines, can be effective, they also carry risks of dependency and sedation. Ketamine offers a non-addictive alternative that can provide relief without the potential for dependence. For individuals who experience debilitating anxiety that disrupts daily life, ketamine’s rapid onset can provide immediate relief, offering a new approach to managing symptoms when conventional treatments fall short.
5. Recreational Use, Misuse, and Potential Risks
Despite its promising medical applications, ketamine has a history of recreational misuse due to its dissociative and hallucinogenic effects. Known on the street as “Special K,” ketamine can produce intense euphoria, visual distortions, and a feeling of detachment from reality. Recreational users typically administer ketamine in unregulated doses, often via injection or inhalation, leading to unpredictable effects and potential health risks. High doses can induce a state known as the “K-hole,” a deeply dissociative experience that can be distressing and disorienting.
Misuse of ketamine can lead to physical and psychological dependence. Chronic, high-dose use is associated with health risks such as bladder toxicity, cognitive impairment, and memory issues. Ketamine’s status as a Schedule III controlled substance in the United States reflects its potential for abuse and its medical applications, making it legally available only through prescription or in licensed medical settings.
Controlled medical use of ketamine minimizes these risks by adhering to strict dosing and monitoring protocols. When administered in a clinical setting, ketamine is given in carefully regulated doses, with healthcare providers monitoring vital signs and ensuring patient safety. Patients are typically screened for any history of substance misuse or psychiatric conditions that might contraindicate ketamine use. While ketamine has proven to be safe and effective when administered correctly, patients should be aware of potential side effects, such as nausea, dizziness, or mild hallucinations, which are usually temporary and manageable under medical supervision.
6. The Future of Ketamine Therapy and Ongoing Research
Ketamine’s effectiveness in treating treatment-resistant conditions has spurred ongoing research aimed at understanding and expanding its potential applications. Researchers are investigating whether ketamine could be used for other mental health conditions, such as bipolar disorder and obsessive-compulsive disorder (OCD), as well as exploring optimal dosing protocols to maximize benefits and minimize risks. In some studies, ketamine has shown potential for promoting resilience against stress and preventing the development of PTSD in trauma survivors, suggesting it may have preventive as well as therapeutic uses.
One of the most exciting areas of research is in ketamine-assisted psychotherapy (KAP). KAP involves the administration of ketamine in conjunction with psychotherapy sessions, using ketamine’s effects to facilitate openness and emotional insight. This approach is gaining traction among clinicians and patients who believe ketamine’s dissociative properties enhance therapeutic breakthroughs. While more research is needed to validate its efficacy, KAP has shown promising results in treating complex cases of depression, PTSD, and anxiety.
Ketamine has also paved the way for further research into rapid-acting antidepressants and the development of drugs that work through similar mechanisms. As understanding of ketamine’s impact on neural pathways grows, it is likely to inform the creation of new therapies for mental health and pain management. In many ways, ketamine is revolutionizing how medical professionals approach treatment-resistant conditions, offering hope to individuals who have struggled with conventional medications.
Conclusion
Ketamine is a unique and versatile medication that has evolved from its origins as an anesthetic to become a powerful tool in the treatment of chronic pain, depression, PTSD, and anxiety. Its rapid action on the NMDA receptor and secondary effects on neurotransmitters make it especially valuable for conditions resistant to standard therapies, providing quick relief that is crucial for patients in acute distress. While ketamine’s potential for misuse and dependency necessitates controlled medical administration, its therapeutic benefits cannot be overlooked. The emergence of ketamine-assisted psychotherapy and other innovative applications underscores the drug’s potential to redefine mental health and pain management.
As research continues, ketamine may unlock new pathways for understanding and treating complex conditions, expanding its use in a safe and controlled manner. While not without risks, when used responsibly under medical supervision, ketamine offers hope and relief to individuals who have long sought effective treatment. Whether as an anesthetic, a pain reliever, or a mental health therapy, ketamine’s impact on modern medicine is profound, providing a valuable addition to the arsenal of treatments available to those in need.