Infection and inflammation are two essential processes within the body, each playing a critical role in our response to injury, disease, and overall health management. While the terms are often used interchangeably, they describe distinct biological phenomena with separate causes, mechanisms, and implications. Understanding the key differences between infection and inflammation can provide valuable insights into how the body combats various threats, allowing for more informed health decisions and targeted treatments.
Infection is primarily caused by external agents such as bacteria, viruses, fungi, or parasites, which invade the body, multiply, and cause harm. Inflammation, however, is a complex response initiated by the immune system to protect and repair tissues affected by infection, injury, or other triggers. Although inflammation often accompanies infection, not all inflammation results from infection, as it can be triggered by other factors such as allergens, autoimmune disorders, or physical injury. Recognizing these distinctions can help in identifying symptoms, understanding health conditions, and choosing the right medical interventions.
Defining Infection: Causes and Mechanisms
Infection occurs when pathogens—organisms such as bacteria, viruses, fungi, or parasites—enter the body, evade its defenses, and begin to reproduce. These microorganisms use various methods to breach the body’s barriers, infiltrating tissues and potentially reaching the bloodstream or other organs. Once inside, these pathogens disrupt normal cellular processes, either by damaging cells directly, releasing toxins, or hijacking cell machinery to reproduce.
There are four main types of infections based on the pathogen involved:
- Bacterial Infections: Bacteria are single-celled organisms that thrive in various environments, from soil to the human body. Bacterial infections can affect nearly every bodily system, with examples including strep throat, urinary tract infections, and bacterial pneumonia. Antibiotics are commonly used to treat bacterial infections, as these drugs specifically target bacterial cells without harming human cells.
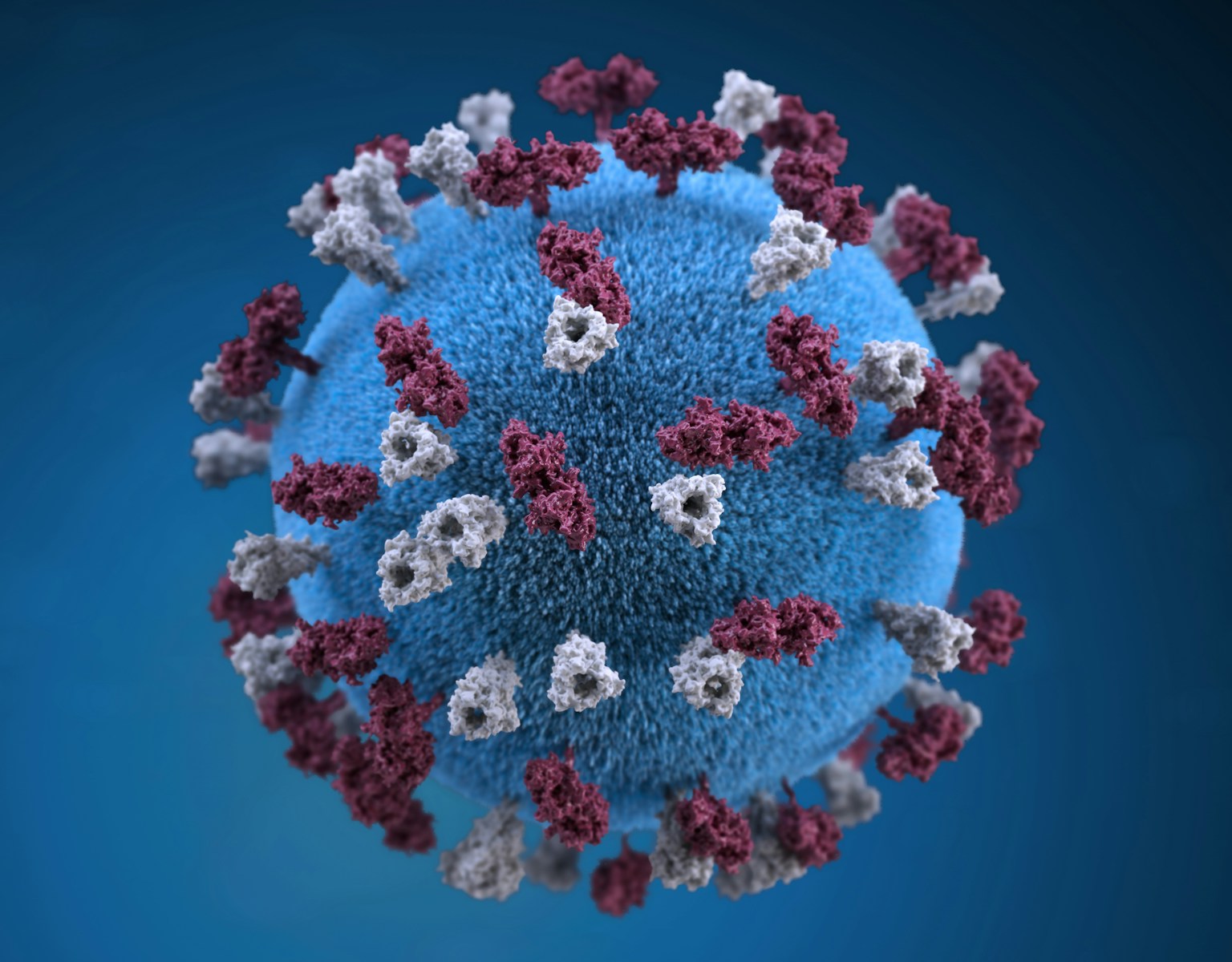
- Viral Infections: Viruses are much smaller than bacteria and require a host cell to reproduce. After entering the body, viruses invade cells and use their machinery to replicate. Viral infections include the flu, HIV, and COVID-19. Since viruses hide within cells, they can be difficult for the immune system to detect and eliminate, making some viral infections challenging to treat. Antiviral medications may slow the virus, but many viral infections rely on the immune system’s ability to clear the infection naturally.
- Fungal Infections: Fungi, including yeasts and molds, can also invade the body, typically affecting skin, nails, or lungs. Fungal infections include athlete’s foot, ringworm, and systemic candidiasis. Antifungal medications, both topical and oral, are used to treat these infections, targeting the unique components of fungal cells.
- Parasitic Infections: Parasites such as protozoa and worms can cause infections, often affecting the gastrointestinal system, blood, or other organs. Malaria, caused by protozoan parasites, and giardiasis, a common intestinal infection, are examples of parasitic infections. These infections typically require antiparasitic medications and may have more complex treatment protocols.
Infections cause a variety of symptoms, influenced by the type of pathogen and the location of the infection. Common signs include fever, fatigue, muscle aches, and localized pain, which result from the immune system’s attempts to neutralize the invaders. The severity of an infection depends on factors like the pathogen’s virulence, the infected area, and the strength of the host’s immune system.
Understanding Inflammation: Causes and Process
Inflammation is a complex immune response aimed at protecting the body from injury or harmful stimuli. Unlike infection, which originates from an external pathogen, inflammation is the body’s internal reaction to threats, which can include infection, but also allergens, irritants, toxins, or physical injury. Inflammation is, in essence, the body’s repair mechanism, mobilizing immune cells, blood flow, and various signaling molecules to the affected site to combat harmful agents and initiate tissue healing.
The inflammatory response is divided into four stages:
- Recognition of Harmful Stimuli: When the immune system detects harmful agents or injury, immune cells like macrophages and dendritic cells identify foreign substances, damaged cells, or invading pathogens, which sets the stage for an inflammatory response.
- Activation of Immune Cells: Upon recognizing a threat, immune cells release signaling proteins called cytokines and chemokines. These molecules act as chemical signals, alerting other immune cells to migrate to the affected area.
- Vasodilation and Increased Permeability: Blood vessels in the affected area dilate and become more permeable, allowing immune cells, fluids, and proteins to reach the injured or infected tissues. This causes characteristic symptoms of inflammation, such as redness, warmth, swelling, and pain.
- Elimination of Harmful Agents and Tissue Repair: The immune cells work to neutralize the cause of the inflammation, whether it’s a pathogen or a damaged cell, and subsequently initiate tissue repair. Once the repair is complete, inflammation usually subsides.
Inflammation can be classified into two main types: acute and chronic. Acute inflammation occurs suddenly and is usually short-lived, lasting from a few hours to a few days. It is a beneficial response that facilitates healing and prevents the spread of harmful agents. Chronic inflammation, however, persists over a longer period and may become harmful. This type of inflammation can result from ongoing exposure to an irritant or an autoimmune disorder, where the immune system mistakenly targets healthy cells. Chronic inflammation has been linked to various health conditions, including heart disease, diabetes, arthritis, and certain cancers.
Infection vs. Inflammation: Key Differences and Interactions
While infection and inflammation can occur simultaneously, they are distinct in origin and function. Infection is the invasion of the body by harmful microorganisms, whereas inflammation is the body’s defensive response to injury or harmful stimuli. Infections often trigger inflammation as the immune system recognizes and responds to the invading pathogen. However, inflammation can occur independently, without any infectious agent, in cases of physical injury, autoimmune responses, or exposure to irritants.
In the case of infection-triggered inflammation, the immune response works to neutralize both the pathogen and the associated tissue damage. For example, bacterial infections can cause localized inflammation as immune cells target the affected area, leading to symptoms like redness, swelling, and pain. The inflammatory process, in turn, supports the immune system in eliminating the pathogen. While acute inflammation helps clear the infection and repair tissue, chronic inflammation, if unregulated, can exacerbate tissue damage, leading to additional health complications.
Chronic inflammation, which may be unrelated to infection, is a risk factor for numerous health issues. Conditions such as arthritis, asthma, and inflammatory bowel disease (IBD) are characterized by prolonged inflammation that targets otherwise healthy tissues, leading to pain, discomfort, and compromised function. Unlike infection-based inflammation, these conditions require specific treatment approaches aimed at modulating immune responses rather than eliminating pathogens.
Signs and Symptoms: Differentiating Infection and Inflammation
Recognizing the signs of infection versus inflammation is essential for effective diagnosis and treatment. Infections typically produce symptoms related to the specific pathogen, such as fever, chills, body aches, and localized pain or pus in bacterial infections. Viral infections may cause symptoms like fatigue, cough, and a runny nose, while fungal infections often present with skin irritation or respiratory issues, depending on the site of infection. Parasites, depending on the type, may cause symptoms like abdominal pain, diarrhea, or skin lesions.
Inflammation presents with hallmark symptoms that include redness, warmth, swelling, and pain, often localized to the affected area. For example, if inflammation is in a joint, it may lead to swelling and discomfort, while inflammation in the skin may result in redness and tenderness. In cases of chronic inflammation, symptoms may be subtler and include fatigue, low-grade fever, and joint stiffness, particularly in inflammatory conditions like rheumatoid arthritis or lupus.
In instances where inflammation and infection co-occur, such as in bacterial infections, both sets of symptoms may be present. A person with a bacterial infection may experience systemic signs of infection, such as fever, in addition to localized inflammation marked by swelling and redness.
Treatment Approaches: Infection and Inflammation
Since infection and inflammation stem from different causes, treatment approaches vary depending on the underlying condition. Infections require targeted treatments to eliminate the pathogenic organism. For bacterial infections, antibiotics are commonly prescribed to target and kill bacteria. Antiviral medications may be used for specific viral infections, though many viral illnesses resolve on their own as the immune system clears the virus. Fungal infections are treated with antifungal medications, while parasitic infections often require antiparasitic drugs. Proper diagnosis of the pathogen type is essential to choose the right treatment and avoid complications like antibiotic resistance.
Inflammation, on the other hand, may require anti-inflammatory medications to manage symptoms, particularly if the inflammation is chronic or causing significant discomfort. Over-the-counter medications like nonsteroidal anti-inflammatory drugs (NSAIDs) can reduce pain and swelling in cases of acute inflammation, while corticosteroids may be prescribed for chronic inflammatory conditions. In cases of autoimmune disorders, immunosuppressants may be used to regulate the immune response and minimize tissue damage. Lifestyle changes, such as a balanced diet, regular exercise, and stress management, also play a vital role in managing chronic inflammation, as they reduce inflammation triggers within the body.
Prevention and Health Management
Preventing infections involves maintaining good hygiene, receiving appropriate vaccinations, and practicing safe food handling and sanitation measures. Washing hands frequently, avoiding close contact with sick individuals, and boosting immune health through a nutrient-rich diet all contribute to reducing infection risks. Vaccinations play an essential role in preventing infections by providing immunity against specific pathogens, especially in vulnerable populations.
For preventing and managing inflammation, lifestyle factors are equally important. A diet rich in anti-inflammatory foods, such as fruits, vegetables, whole grains, and healthy fats, can reduce the risk of chronic inflammation. Physical activity, adequate sleep, and stress reduction also support immune health and reduce inflammation. In individuals with chronic inflammatory conditions, working with healthcare professionals to develop a personalized treatment plan is essential for managing symptoms and minimizing flare-ups.
Understanding the differences between infection and inflammation allows individuals to recognize symptoms, seek timely medical care, and adopt preventive measures that support health. Although infection and inflammation often interact, their distinct characteristics underscore the importance of tailored treatment approaches for each condition. By recognizing and addressing these processes appropriately, we can take proactive steps toward optimal health and well-being.