Pain is a complex and multifaceted sensation that serves a crucial role in our survival and well-being. It is a vital mechanism that alerts us to potential harm or injury, prompting us to take appropriate action to protect ourselves. At a biological level, pain involves a complex interplay of sensory signals, neurotransmitters, and neural pathways that transmit and process information from the site of injury to the brain. Pain perception is not only a physical experience but also influenced by psychological and emotional factors, making it a truly intricate phenomenon.
Biological Mechanisms of Pain
When tissue is damaged or injured, specialized nerve endings called nociceptors detect the stimuli and convert them into electrical impulses. These impulses are then transmitted along nerve fibers to the spinal cord and eventually reach the brain, where they are interpreted as pain. Neurotransmitters such as glutamate and substance P play a key role in transmitting these pain signals between nerve cells. Additionally, the brain’s interpretation of pain can be modulated by factors like attention, mood, and past experiences, highlighting the complexity of the pain experience.
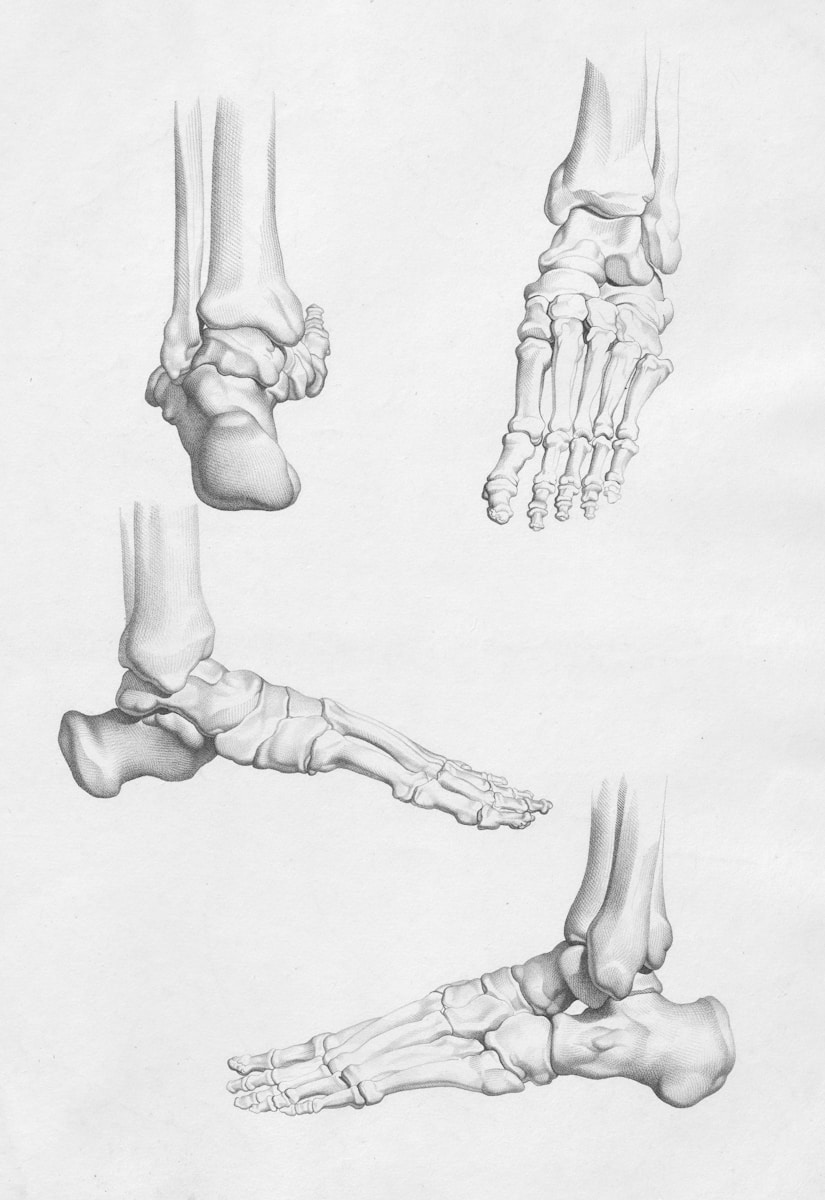
The Role of Nociceptors
Nociceptors are specialized receptors located throughout the body, particularly in the skin, joints, and organs. They come in various types, each responsive to different stimuli such as thermal, mechanical, or chemical changes. For instance, when you accidentally touch a hot stove, thermal nociceptors are activated, sending signals through A-delta fibers, which are myelinated and transmit sharp, immediate pain. Understanding these pathways helps in developing targeted therapies, such as local anesthetics, which can block nerve conduction and reduce pain.
Neurotransmitter Dynamics
The neurotransmitter dynamics in pain perception are intricate. For example, while glutamate is an excitatory neurotransmitter that facilitates the transmission of pain signals, gamma-aminobutyric acid (GABA) serves as an inhibitory neurotransmitter that can modulate pain by dampening these signals. This balance between excitatory and inhibitory neurotransmitters is crucial, as an imbalance can lead to heightened pain sensitivity, a condition known as hyperalgesia. This understanding has led to treatments such as GABA analogs for neuropathic pain management.
Protective Function of Pain
One of the primary functions of pain is to protect the body from further harm. The experience of pain prompts immediate behavioral responses, such as withdrawal from a hot surface or seeking medical attention for a serious injury. By alerting us to potential threats, pain helps us avoid dangerous situations and take necessary precautions to prevent further damage. Pain not only serves as a warning signal but also initiates adaptive responses that are crucial for our survival and well-being.
Pain as a Learning Tool
Pain also functions as a critical learning tool, discouraging behaviors that could result in injury. Take, for example, a child who touches a cactus. The sharp pain teaches them to avoid such contact in the future, thereby preventing repeated harm. In more severe cases, such as a sprained ankle, the immediate pain encourages rest, which is essential for healing.
Adaptive Responses
The body’s adaptive responses to pain include increased blood flow and immune activity to the affected area, promoting healing. Techniques such as the RICE method (Rest, Ice, Compression, Elevation) are practical applications that leverage the body’s natural response to pain, aiding in faster recovery from injuries like sprains and strains.
Role of Inflammation in Pain
Inflammation is a common response to tissue injury and plays a significant role in the generation of pain. Inflammatory mediators released at the site of injury sensitize the nociceptors, making them more responsive to painful stimuli. This heightened sensitivity amplifies the perception of pain and contributes to the protective response by promoting rest and healing of the affected area. Inflammation-induced pain mechanisms are an essential part of the body’s defense and repair processes, highlighting the intricate interplay between inflammatory responses and pain perception.
Inflammatory Mediators
Key players in inflammation include prostaglandins, cytokines, and bradykinin. These substances not only increase nociceptor sensitivity but also cause vasodilation and swelling, which can further exacerbate pain. Over-the-counter medications like NSAIDs (non-steroidal anti-inflammatory drugs) work by inhibiting the production of prostaglandins, thereby reducing inflammation and pain.
Chronic Inflammation
Chronic inflammation can have lasting effects on pain perception. Conditions such as rheumatoid arthritis demonstrate how prolonged inflammation leads to persistent pain and joint damage. Understanding these processes has led to the development of disease-modifying antirheumatic drugs (DMARDs), which target the inflammatory pathways more directly.
Chronic Pain and Maladaptive Responses
While acute pain is essential for our survival, chronic pain can have maladaptive effects on our well-being. Conditions such as persistent pain can lead to physical and psychological consequences, impacting our quality of life and overall functioning. Understanding the underlying mechanisms of chronic pain is crucial for developing targeted interventions to alleviate suffering and improve the lives of individuals affected by long-term pain. Chronic pain can result in changes in the nervous system, leading to increased sensitivity to pain stimuli and maladaptive pain behaviors that perpetuate the pain experience.
Neuropathic Pain
One form of chronic pain is neuropathic pain, which arises from damage to the nerves themselves. This type of pain is often described as a burning or shooting sensation and can result from conditions such as diabetes or shingles. Treatments like anticonvulsants and antidepressants are often used to manage neuropathic pain, as they modulate the neurotransmitter systems involved in pain signaling.
Psychological Impact
Chronic pain doesn’t just affect the body; it has profound psychological impacts. Individuals with chronic pain often experience anxiety, depression, and sleep disturbances. Cognitive-behavioral therapy (CBT) has been proven effective in managing the psychological aspects of chronic pain, helping individuals develop coping strategies and improve their quality of life.
Pain Management Strategies
Effective pain management often requires a multidisciplinary approach, incorporating physical therapy, medications, and psychological support. For instance, physical therapy can help restore function and reduce pain through exercises tailored to the individual’s condition, while psychological interventions can address the emotional toll of living with chronic pain.
Future Directions in Pain Research
The quest to understand and manage pain continues to evolve. Advances in genetics and neuroscience have opened new avenues for research, offering hope for more personalized pain management strategies. For example, genetic studies have identified specific variations that may influence pain sensitivity and response to medications, paving the way for tailored treatments.
Cutting-edge Technologies
Emerging technologies such as neuroimaging and biofeedback offer new insights into pain processing and regulation. These tools can help visualize how different brain regions communicate during pain experiences, potentially leading to innovative therapies that target specific neural circuits.
Personalized Medicine
The future of pain management may lie in personalized medicine, where treatments are tailored to an individual’s genetic makeup, lifestyle, and environmental factors. This approach promises to enhance the efficacy of pain management strategies and minimize side effects.
Common Mistakes in Pain Management
Despite advances in understanding pain, common mistakes persist in its management. Over-reliance on opioids, for instance, has led to an epidemic of addiction and overdose. It’s crucial to explore alternative treatments and emphasize comprehensive pain management plans that address both physical and psychological aspects.
Avoiding Overmedication
One mistake is the overuse of pain medications without considering underlying causes or alternative therapies. Patients should be encouraged to discuss non-pharmacological treatments with their healthcare providers, such as physical therapy, acupuncture, or mindfulness practices, which can help manage pain without the side effects associated with long-term medication use.
Importance of Accurate Diagnosis
Misdiagnosis or delayed diagnosis of the underlying cause of pain can lead to ineffective treatment. Comprehensive assessment by a multidisciplinary team can ensure accurate diagnosis and more effective management strategies.
Pain is a sophisticated biological process that serves a crucial role in protecting our bodies from harm and ensuring our survival. By unraveling the intricate mechanisms underlying pain perception and response, researchers and healthcare providers can develop more effective strategies for managing pain and improving the well-being of individuals experiencing acute or chronic pain. It is essential to consider pain as a multidimensional experience, encompassing biological, psychological, and social factors, in order to provide comprehensive and personalized pain management approaches that address the complexity of pain perception and response.