The human brain, as the most metabolically active organ in the body, generates substantial amounts of metabolic waste during its processes of cognition, homeostasis, and systemic regulation. Despite its complexity and importance, the brain conspicuously lacks a traditional lymphatic system, raising a critical question: how does it efficiently clear these metabolic byproducts? The answer lies in the glymphatic system, an innovative discovery that has profoundly influenced the fields of neuroscience and physiology.
This system, active predominantly during sleep, facilitates the removal of neurotoxic waste and ensures optimal cerebral function. Its efficient operation is vital for maintaining brain health, preventing neurological decline, and mitigating the risks associated with aging and neurodegenerative diseases. As researchers uncover its mechanisms, the glymphatic system emerges as a cornerstone in understanding neurological health, the aging process, and diseases such as Alzheimer’s.
In this article, we’ll take a look at the intricate dynamics of this self-cleansing system to uncover the critical interplay between sleep, brain maintenance, and overall cerebral homeostasis.
What is the Glymphatic System?
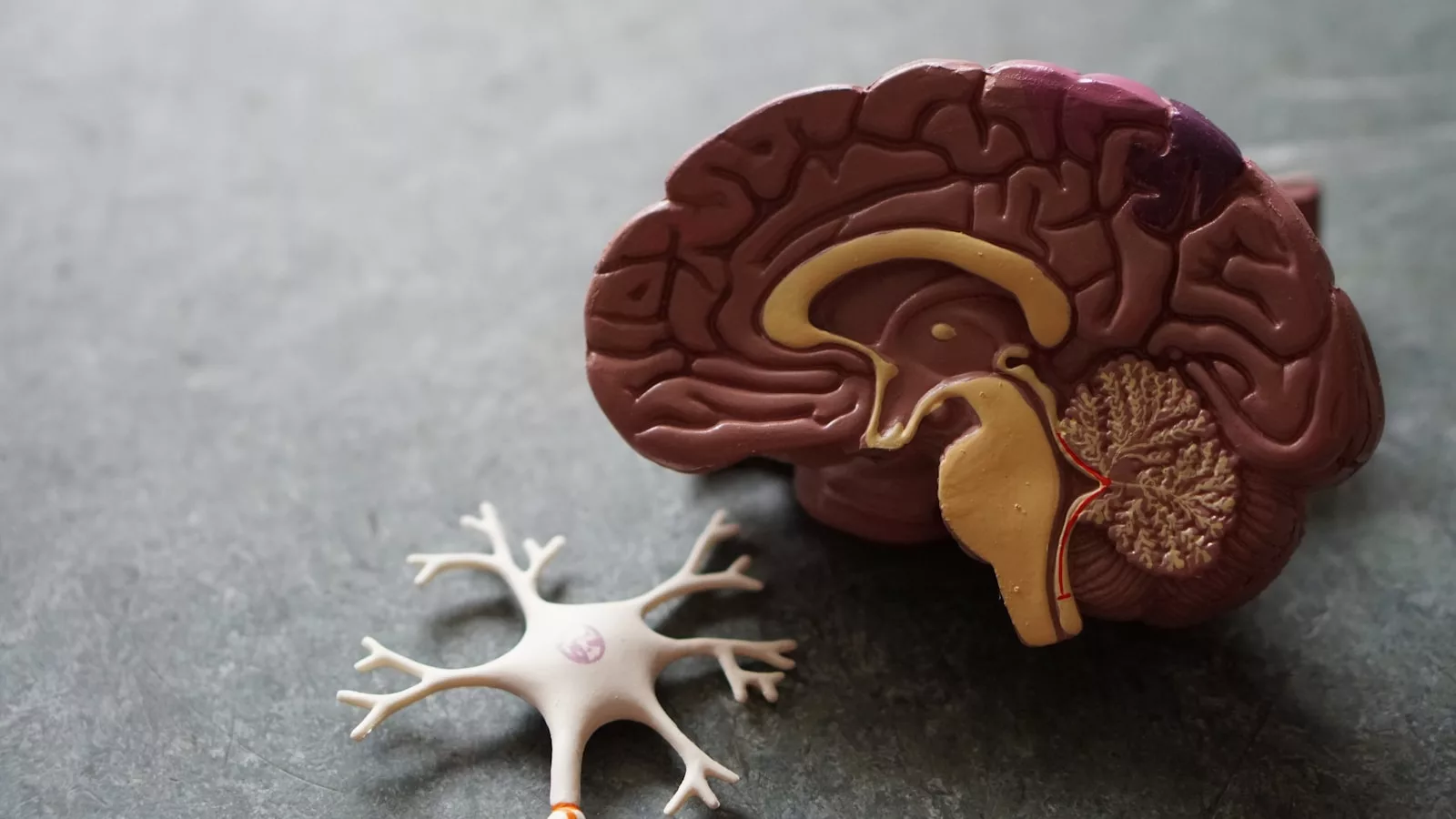
First described in 2012 by Maiken Nedergaard and her colleagues, the glymphatic system is a unique waste clearance pathway in the brain. Operating analogously to the lymphatic system in the rest of the body, it facilitates the removal of cellular waste and the distribution of vital nutrients. The term “glymphatic” integrates the words “glial”—highlighting the pivotal role of glial cells—and “lymphatic,” underscoring its functional similarities to peripheral lymphatic mechanisms.
Anatomy of the Glymphatic System
- Perivascular Pathways: The glymphatic system relies on perivascular conduits surrounding cerebral blood vessels. These pathways enable the flow of cerebrospinal fluid (CSF) into the brain’s interstitial spaces, where it mixes with interstitial fluid (ISF) to remove cellular debris. These channels act as highways for fluid movement, critical for maintaining a clean and functional neural environment.
- Aquaporin-4 (AQP4) Channels: Astrocytes, a class of glial cells, play a central role in this system. Their endfeet, enriched with AQP4 water channels, regulate the exchange of CSF and ISF, ensuring effective fluid dynamics for waste clearance. This molecular mechanism underscores the efficiency of the glymphatic system in managing brain homeostasis.
- Lymphatic Drainage: After traversing the glymphatic pathways, waste products exit the brain via meningeal lymphatic vessels and are subsequently processed by the body’s peripheral lymphatic system. This integration underscores the systemic nature of cerebral waste management, linking the brain’s internal processes to the broader physiological framework.
Primary Functions
The glymphatic system serves two foundational roles:
- Waste Clearance: It removes neurotoxic substances, including amyloid-beta and tau proteins, whose accumulation is implicated in Alzheimer’s disease and other neurodegenerative disorders. Without efficient clearance, these toxins compromise neuronal function and accelerate cognitive decline.
- Nutrient Transport: Beyond waste elimination, this system facilitates the distribution of essential compounds, such as glucose and lipids, necessary for neuronal function and repair. This dual role highlights the glymphatic system’s importance in sustaining neural health and resilience.
The Connection Between Sleep and Glymphatic Activity
The glymphatic system exhibits peak activity during sleep, particularly during non-rapid eye movement (non-REM) sleep stages. This temporal specificity underscores the critical interplay between rest and cerebral homeostasis.
Sleep-Dependent Clearance
- Neuronal Shrinkage: During sleep, neurons reduce in volume by approximately 60%, expanding the interstitial spaces. This morphological adaptation enhances CSF-ISF exchange and facilitates efficient toxin removal. The temporary shrinkage of neurons exemplifies the dynamic adaptability of brain structures during sleep.
- Increased CSF Dynamics: Non-REM sleep significantly boosts cerebrospinal fluid circulation, enabling the removal of metabolic byproducts that accumulate during wakefulness. Enhanced circulation ensures the timely clearance of waste, protecting neural networks from prolonged exposure to toxins.
- Suppressed Neural Activity: Sleep-induced reductions in synaptic firing allow the glymphatic system to operate without competition, prioritizing detoxification processes. This focused activity during sleep demonstrates the brain’s strategic allocation of resources to maintenance tasks.
Consequences of Sleep Deprivation
Chronic sleep deprivation markedly impairs glymphatic efficiency, leading to the progressive accumulation of neurotoxic proteins such as amyloid-beta. This dysfunction has been correlated with:
- Increased susceptibility to Alzheimer’s and Parkinson’s diseases, underscoring the link between disrupted glymphatic activity and neurodegeneration.
- Declines in cognitive performance, memory retention, and executive function, reflecting the immediate effects of inadequate brain maintenance.
- Accelerated neurobiological aging and heightened oxidative stress, further amplifying the risks associated with insufficient sleep.
Implications for Neurological Health
The glymphatic system’s functionality is inextricably linked to neurological well-being. Its impairment has been implicated in a spectrum of pathological conditions, highlighting its importance in both preventative and therapeutic contexts.
Alzheimer’s Disease
The glymphatic system’s role in clearing amyloid-beta plaques and tau protein tangles positions it as a critical player in Alzheimer’s pathology. Dysfunctions in this clearance mechanism exacerbate the deposition of these neurotoxic proteins, accelerating disease progression. Enhancing glymphatic activity through sleep optimization, pharmacological interventions, or targeted therapies offers a promising avenue for mitigating Alzheimer’s risk and improving patient outcomes.
Traumatic Brain Injury (TBI)
Traumatic brain injuries disrupt glymphatic pathways, impairing waste removal and prolonging neuroinflammation. This dysfunction contributes to cognitive deficits and increases the risk of chronic traumatic encephalopathy (CTE). Targeted therapies aimed at restoring glymphatic efficiency could significantly improve post-TBI recovery outcomes, highlighting the system’s therapeutic potential.
Aging and Cognitive Decline
Aging is accompanied by a natural decline in glymphatic activity, rendering the brain more susceptible to oxidative damage and waste accumulation. This decline is implicated in age-related cognitive impairments and neurodegeneration. Strategies to bolster glymphatic function—through lifestyle modifications, emerging medical interventions, and technological advancements—hold potential for preserving cognitive health in aging populations and extending healthy lifespans.
Strategies to Enhance Glymphatic Function
Maintaining glymphatic integrity necessitates a multifaceted approach encompassing lifestyle adjustments, sleep enhancement, and targeted therapeutic measures. Below are key strategies:
1. Optimize Sleep Quality
Prioritizing sleep is foundational to glymphatic efficacy. Recommendations include:
- Consistent Sleep Schedules: Adhering to regular sleep-wake cycles reinforces circadian rhythms, optimizing restorative processes and glymphatic activity.
- Sleep Environment: A cool, dark, and quiet bedroom facilitates deep, uninterrupted sleep, essential for glymphatic function.
- Pre-Sleep Hygiene: Minimizing screen exposure and caffeine intake in the evening supports melatonin production and sleep onset, ensuring optimal rest.
2. Sleep Position
Research indicates that lateral (side) sleeping positions enhance glymphatic flow compared to supine (back) or prone (stomach) positions. This alignment optimizes CSF dynamics, bolstering waste clearance and exemplifying how subtle behavioral changes can significantly impact brain health.
3. Hydration
Adequate hydration is essential for maintaining CSF-ISF fluid balance. While drinking sufficient water throughout the day is critical, excessive nighttime hydration should be avoided to prevent sleep interruptions. Hydration supports the physiological processes underpinning glymphatic efficiency.
4. Physical Activity
Regular exercise enhances cardiovascular health and cerebral circulation, indirectly supporting glymphatic function. Activities such as aerobic workouts, yoga, and brisk walking are particularly beneficial, promoting systemic health and reinforcing the brain’s self-cleaning capabilities.
5. Moderation of Alcohol and Caffeine
Both alcohol and caffeine adversely affect sleep architecture and glymphatic efficiency. Limiting these substances, especially in the hours preceding sleep, is vital for optimal system performance and overall neurological health.
Emerging Research and Future Directions
The burgeoning field of glymphatic research continues to unveil novel insights and therapeutic possibilities. Key areas of exploration include:
Pharmacological Advances
Drugs targeting aquaporin-4 channels are under investigation for their potential to enhance glymphatic flow. Such pharmacological interventions hold promise for treating conditions like Alzheimer’s disease, traumatic brain injury, and age-related cognitive decline.
Advanced Imaging Technologies
Innovations in neuroimaging, including high-resolution MRI and molecular tracers, are enabling detailed visualization of glymphatic activity. These tools facilitate early detection of dysfunction, improved diagnosis of neurodegenerative diseases, and the evaluation of therapeutic efficacy.
Personalized Medicine
Tailoring interventions based on individual variations in glymphatic efficiency could revolutionize preventative and therapeutic strategies. Personalized approaches integrating genetic predispositions, lifestyle factors, and environmental influences may optimize outcomes, paving the way for a new era in brain health management.
Final Words
The glymphatic system represents a pivotal mechanism in maintaining cerebral homeostasis, underscoring the vital interplay between sleep, brain health, and overall well-being. By efficiently clearing metabolic waste and delivering essential nutrients, this system safeguards cognitive function and mitigates the risk of neurodegenerative diseases. Emphasizing sleep quality, hydration, and physical activity, while curbing detrimental habits, provides actionable pathways to enhance glymphatic performance. As scientific inquiry advances, the potential to harness this system for therapeutic innovation continues to grow, offering transformative implications for both individual and public health.