Imagine a life where you never feel pain—an existence where the sting of a cut or the throb of a headache is absent. While this might initially sound like a blessing, for those with congenital insensitivity to pain (CIP), it presents a unique set of challenges. Pain, often perceived as an unwelcome visitor, serves critical roles in safeguarding our health by alerting us to harm and prompting protective reflexes. Despite its undesirable nature, pain is a crucial biological tool that promotes healing and prevents further injury. This article dives deep into the enigma of CIP, exploring the genetic quirks that lead to this rare condition and the broader implications for pain research and management.
Understanding Pain: The Body’s Alarm System
To appreciate the rarity and implications of CIP, we first need to understand how pain functions in the human body. Pain is not just a simple sensation; it’s a complex interplay of signals and perceptions that involve both physical and emotional components.
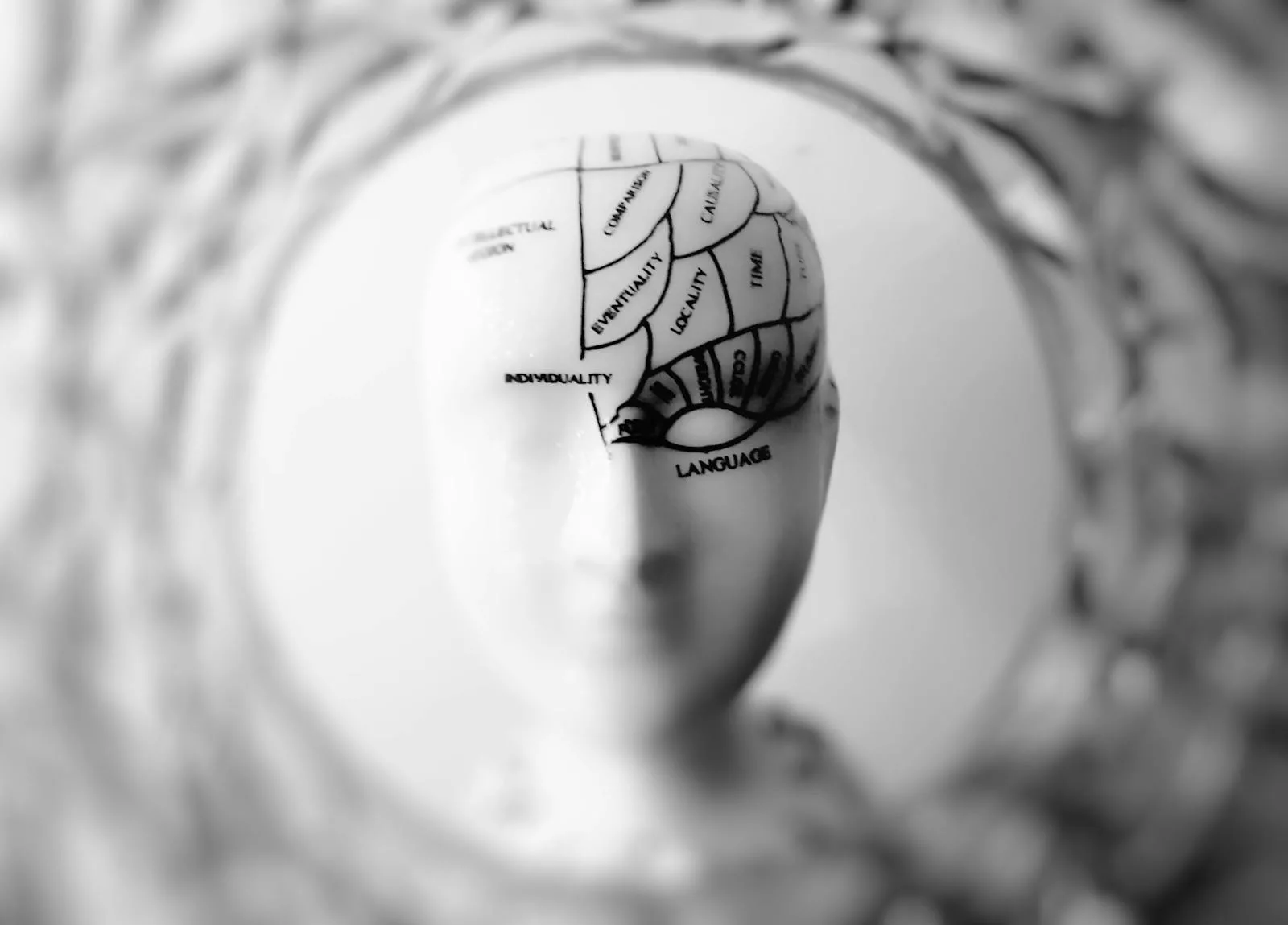
The Mechanics of Pain Perception
At its core, pain begins with specialized nerve endings known as nociceptors. These are strategically distributed throughout the body—particularly in the skin, muscles, and internal organs—to detect potentially harmful stimuli like sharp objects, extreme temperatures, or toxic chemicals. Upon encountering such stimuli, nociceptors generate electrical impulses that travel through peripheral nerves to the spinal cord and ultimately reach the brain. It is here that these signals are interpreted as pain, prompting a response to mitigate or avoid injury.
The Pain Pathway
The journey of a pain signal is a marvel of biological efficiency. When a nociceptor activates, it sends an impulse along sensory neurons to the dorsal horn of the spinal cord. From there, the signal is relayed to ascending pathways that carry it to various brain regions, including the thalamus and cerebral cortex, where it’s processed and perceived as pain. This complex network ensures that the body can react swiftly to potential threats, often before we’re consciously aware of them.
The Role of Context and Emotion
Pain perception is highly subjective, influenced by an individual’s emotional state, context, and past experiences. This is why two people might react differently to the same painful stimulus. For instance, athletes often endure pain differently during competition, driven by adrenaline and focus, compared to their response in a neutral setting. This subjectivity plays a crucial role in pain management and treatment, as it highlights the importance of addressing both physical and emotional factors in care plans.
Congenital Insensitivity to Pain: A Disruption in the System
For individuals with CIP, the normal pathway of pain perception is disrupted. This absence of pain is not due to a lack of injury, but rather a breakdown in the communication system that alerts the brain to potential harm.
The Genetic Puzzle
CIP is extremely rare, with only a few hundred documented cases worldwide. The condition is typically inherited, stemming from genetic mutations that affect the nervous system’s ability to process pain. Three primary genes have been identified as culprits: SCN9A, SCN11A, and PRDM12.
SCN9A and Nav1.7 Channels
The most extensively studied genetic cause of CIP involves mutations in the SCN9A gene, which encodes the Nav1.7 sodium channel. These channels are vital for the generation and transmission of pain signals. Mutations here can render these channels non-functional, silencing the nociceptors and preventing pain signals from reaching the brain. Interestingly, different mutations in the same gene can lead to opposite conditions, such as extreme pain sensitivity, illustrating the intricate balance required for normal sensory function.
Other Genetic Influences: SCN11A and PRDM12
Beyond SCN9A, mutations in the SCN11A gene, which encodes the Nav1.9 sodium channel, can also lead to CIP. These mutations cause the channels to be overactive, paradoxically dampening pain signal transmission. Similarly, mutations in PRDM12, which is crucial for the development and maintenance of nociceptors, can result in an absence of functional pain-sensing neurons.
The Complexity of Genetic Interactions
It’s essential to recognize that genetic factors interact in complex ways, and not all individuals with mutations in these genes experience CIP. Environmental factors, other genetic elements, and even epigenetic changes may influence whether an individual will manifest the condition. This complexity underscores the challenges researchers face in developing comprehensive models of pain perception and insensitivity.
Living Without Pain: The Hidden Dangers
While a life devoid of pain might initially seem advantageous, it is fraught with significant risks. Individuals with CIP are prone to injuries and health issues that would typically be avoided or promptly addressed due to pain signals.
Childhood Challenges and Adaptations
From a young age, children with CIP may inadvertently harm themselves. A toddler might chew on their lips or fingers without realizing the damage. They might touch hot surfaces or play rough, oblivious to the burns or fractures they are sustaining. Parents and caregivers play a crucial role in minimizing these risks by creating a safer environment and teaching the child to be vigilant about potential hazards.
Practical Safety Measures for Children
Implementing practical safety measures is crucial for children with CIP. This includes using protective gear, such as helmets and knee pads, during play and sports. Parents might also employ temperature-regulating devices to prevent burns and ensure sharp objects are out of reach. Regular skin checks can help identify unnoticed injuries, allowing for prompt medical attention and reducing the risk of infection.
Everyday Risks and Medical Complications
As they grow, individuals with CIP face ongoing challenges. Without pain to signal injury, they might walk on a broken bone or overlook a serious cut, leading to complications like infections or joint deformities. Medical care becomes complex, as pain is a critical indicator for diagnosing illnesses and assessing treatment efficacy. Conditions like appendicitis or heart attacks can go unnoticed until they become severe, underscoring the protective role pain plays in health management.
Strategies for Managing CIP
Despite these challenges, many with CIP adapt by developing heightened awareness of their bodies and surroundings. Regular medical check-ups become essential to catch potential health issues early. Modifying their environment to reduce injury risk and engaging in daily routines to check for unnoticed injuries are practical strategies to manage the condition effectively.
Developing Routine Health Checks
For those with CIP, establishing a routine for health checks can mitigate some risks. Daily inspections for cuts, bruises, or signs of infection, as well as regular visits to healthcare professionals, are vital. Encouraging a habit of mindful observation can help individuals detect changes in their physical state, compensating for the lack of pain signals.
Insights from CIP: Transforming Pain Research
The study of CIP offers profound insights into the biology of pain and potential new avenues for pain management. Traditional pain relief methods, like opioids, often bring undesirable side effects and addiction risks. By understanding the genetic and molecular foundations of CIP, researchers hope to discover safer, targeted treatments.
Targeted Drug Development
One promising direction involves creating drugs that mimic the effects of SCN9A mutations, which could selectively block pain pathways by inhibiting Nav1.7 channels. Such drugs could provide relief for chronic pain sufferers without affecting other sensory functions. Early research indicates that blocking these channels can yield significant analgesic effects, paving the way for more refined pain management strategies.
The Path to New Analgesics
Developing new analgesics based on genetic insights requires extensive research and clinical trials. Researchers aim to create molecules that target specific channels or receptors involved in pain transmission, minimizing side effects and maximizing efficacy. The ultimate goal is to offer chronic pain patients relief without the risk of addiction or other complications associated with current treatments.
The Promise of Genetic Interventions
Gene therapy is another frontier being explored, offering the possibility of long-term relief by directly altering the genes responsible for pain signaling. The understanding gleaned from CIP research also extends to other neurological disorders, highlighting the broader potential impact of these findings.
Ethical Considerations in Gene Therapy
While gene therapy holds promise, it also raises ethical questions. The potential for unintended consequences and the implications of genetic modifications on future generations must be carefully considered. Ongoing dialogue among scientists, ethicists, and the public is crucial to navigate these challenges responsibly.
Broader Implications: Rethinking Pain and Humanity
The existence of individuals who never feel pain challenges our understanding of human experience. Pain, often seen as a mere inconvenience, is integral to learning, empathy, and survival.
Pain as a Teacher and a Connector
Pain teaches us to avoid harm and fosters empathy for others’ suffering. The absence of pain in CIP highlights the complex relationship between sensory perception and emotional development, offering unique insights into human behavior and resilience.
The Ethical and Philosophical Dimensions
CIP prompts profound questions about the necessity of pain and its role in shaping who we are. It challenges researchers and ethicists to consider how pain informs our decisions, interactions, and personal growth.
Moving Forward: The Future of Pain Management
The insights from CIP research hold the potential to revolutionize pain management, offering hope for millions who suffer from chronic pain. As science continues to unravel the genetic and molecular mechanisms of pain, the lessons from CIP may lead to breakthroughs in how we perceive, understand, and treat pain.
Practical Steps for Those with CIP
For individuals with CIP and their caregivers, knowledge is power. Regular health monitoring, environmental safety precautions, and education about the condition are essential steps in managing life without pain. Protective gear, routine body checks, and a proactive approach to healthcare can mitigate some of the risks associated with this unique condition.
Creating a Supportive Community
Building a supportive community is vital for those with CIP. Connecting with others who share similar experiences can provide emotional support and practical advice. Online forums and support groups offer spaces where individuals can share strategies, successes, and challenges, fostering a sense of belonging and understanding.
A New Era in Pain Treatment
The future may hold the promise of targeted therapies that offer pain relief without the drawbacks of current treatments. By leveraging the genetic insights from CIP, we could usher in a new era of pain management that respects the delicate balance of human sensory and emotional experiences.
Collaborative Research and Innovation
Collaboration between geneticists, neurologists, and pharmacologists is essential to harness the full potential of CIP research. By pooling resources and expertise, the scientific community can accelerate the development of novel treatments and improve the quality of life for those suffering from pain disorders.
In exploring CIP, we not only expand our scientific understanding but also deepen our appreciation for the human condition. This journey into the mysteries of pain challenges us to consider its necessity and potential, ultimately guiding us toward a future where pain can be managed more effectively and compassionately.