Gonorrhea is one of those infections people assume they’d recognize and handle quickly—burning urination, a quick shot, done. The reality is more nuanced. Many cases are silent, the throat and rectum can be infected without obvious symptoms, and antibiotic resistance has reshaped treatment in recent years. If you’re sexually active, understanding how gonorrhea spreads, how it’s diagnosed, and what modern treatment looks like is part of basic sexual health literacy. This guide distills current best practices from frontline clinic experience and up-to-date guidance through 2023, so you can protect yourself and the people you care about.
Understanding Gonorrhea
What We’re Talking About When We Talk About Gonorrhea
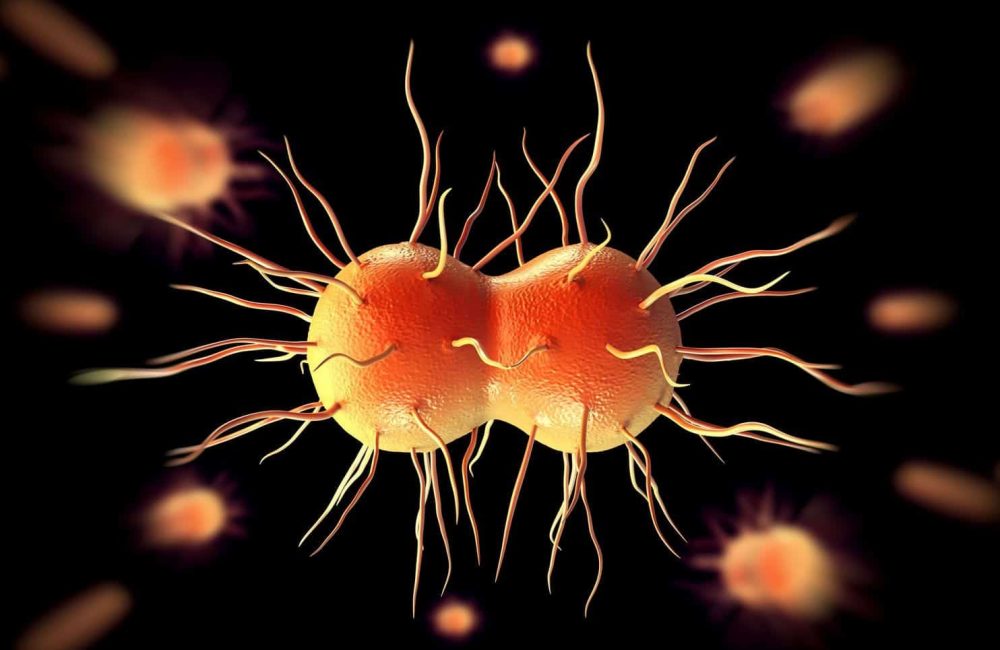
Gonorrhea is caused by Neisseria gonorrhoeae, a bacterium that prefers the mucous membranes of the urethra, cervix, rectum, throat, and eyes. It’s a gram-negative diplococcus, a fancy way of saying that under the microscope it looks like two small coffee beans stuck together. It travels via sexual contact—vaginal, anal, or oral—and from parent to newborn during delivery. It doesn’t live long on dry surfaces and doesn’t spread through toilet seats, pools, or casual contact.
Fast Realities
- The World Health Organization estimates around 82 million new cases of gonorrhea each year worldwide.
- In the U.S., reported cases have climbed over the past decade. Hundreds of thousands of cases are documented annually, and that’s just what’s reported; many infections go undiagnosed.
- A large share of infections have no symptoms—especially in the throat and rectum—so relying on “I feel fine” as a strategy misses a lot.
How Gonorrhea Spreads
Gonorrhea spreads through contact with infected mucous membranes:
- Penis-to-vagina, penis-to-penis, penis-to-anus, penis-to-mouth
- Mouth-to-vagina, mouth-to-penis, mouth-to-anus
- Anus-to-mouth or sharing of sex toys that contact mucosa and aren’t cleaned or covered between partners
- Parent to newborn during vaginal delivery
Practical Clarifications
- Oral Sex: Oral sex can transmit gonorrhea. In clinics, pharyngeal (throat) gonorrhea is common among people who engage in oral sex, often with no throat symptoms at all.
- Condom Use: Condoms reduce risk substantially for vaginal and anal sex, but a lot of exposure happens through unprotected oral sex. Barriers like condoms and dental dams during oral sex are effective and underused.
- Transmission Myths: Hand-to-genital transmission is far less efficient; the bacteria don’t thrive on skin for long. The higher risk comes from direct mucosa-to-mucosa contact. Toilet seats and casual contact aren’t realistic sources of transmission.
Recognizing Symptoms and Silent Infections
What Gonorrhea Looks Like (and When It Doesn’t)
Gonorrhea’s hallmark symptoms vary by site of infection. Incubation is typically 2–7 days for urethral infections in people with penises, and up to about two weeks elsewhere. Symptoms (when they occur) include:
- Urethral (penis): Burning with urination; discharge that’s often white-yellow-green; urethral itching or irritation; sometimes testicular pain if epididymitis develops.
- Cervical/vaginal: Increased discharge; bleeding between periods; post-coital bleeding; pelvic or lower abdominal pain if pelvic inflammatory disease (PID) is present; burning with urination; many are asymptomatic or have mild, nonspecific symptoms.
- Rectal: Discharge, itching, soreness, painful bowel movements, bleeding—or no symptoms at all.
- Throat (pharyngeal): Sore throat, swollen glands—or completely silent.
- Eyes: Conjunctivitis with significant redness, swelling, and discharge—this is uncommon but urgent.
The Silent Part Matters
Pharyngeal and rectal infections are frequently asymptomatic. Among people with vaginas, up to half may not notice clear gonorrhea symptoms. Even among people with penises, early infection sometimes flies under the radar.
Why Untreated Gonorrhea Isn’t “No Big Deal”
The stakes are real:
- Pelvic Inflammatory Disease (PID): Untreated cervical infections can ascend to the uterus and fallopian tubes. PID can cause chronic pelvic pain, increase risk for ectopic pregnancy, and contribute to infertility. Risk estimates vary, but infertility after one episode of PID is often cited around 10%, and the risk rises with repeat episodes.
- Epididymitis: Painful inflammation near the testicle; rare cases can threaten fertility if not treated promptly.
- Disseminated Gonococcal Infection (DGI): Rare but serious spread to the bloodstream causing joint pain, rash, fever, and sometimes severe complications like endocarditis.
- HIV Risk: Gonorrhea increases both susceptibility to and transmissibility of HIV by causing local inflammation and increasing viral shedding. Co-infection management is a key part of care.
The 2023 Treatment Landscape: What Changed and Why
A few years ago, you might have heard about “dual therapy” for gonorrhea: an injection of ceftriaxone plus oral azithromycin. That changed as resistance patterns evolved. By 2020–2021, surveillance showed rising azithromycin resistance and growing concern about antimicrobial stewardship. In response, U.S. guidelines moved to higher-dose ceftriaxone monotherapy for uncomplicated gonorrhea.
Current Standard Treatment
The current standard in the U.S. (and reflected in many countries’ guidance) for uncomplicated cervical, urethral, or rectal gonorrhea in adults and adolescents is:
- Ceftriaxone 500 mg intramuscularly as a single dose for persons weighing under 150 kg (330 lb)
- Ceftriaxone 1 g intramuscularly as a single dose for persons weighing 150 kg (330 lb) or more
- If chlamydial infection hasn’t been ruled out, add doxycycline 100 mg by mouth twice daily for 7 days (azithromycin is used in pregnancy instead of doxycycline)
Why This Regimen?
- Ceftriaxone Remains Reliable: Ceftriaxone remains reliably active.
- Higher Dosing: Higher dosing helps overcome reduced susceptibility.
- Azithromycin Dropped: Azithromycin was dropped from routine dual therapy to reduce selection pressure for resistance.
Pharyngeal infections are trickier to cure, and that’s why a test-of-cure is recommended for throat gonorrhea—more on that in the testing section.
Alternatives for Allergies or Access Issues
If you’re allergic to cephalosporins or can’t access ceftriaxone, there are alternatives, but they come with caveats:
- Gentamicin 240 mg intramuscularly plus azithromycin 2 g by mouth once has been studied as an alternative for urogenital infection in cephalosporin-allergic patients, but GI side effects can be significant, and effectiveness for pharyngeal infection is lower.
- Cefixime 800 mg by mouth once may be used if an injection can’t be given. It’s less effective for pharyngeal infections, and ceftriaxone is preferred when possible.
Considerations for Pregnancy
- Ceftriaxone is Safe: Ceftriaxone is safe and recommended at the same dosing.
- Chlamydia Co-Infection: If chlamydia hasn’t been excluded, use azithromycin 1 g orally once rather than doxycycline.
- Preventing Neonatal Infection: Treating promptly in pregnancy also helps prevent neonatal infection during delivery.
Severe or disseminated infections require IV therapy and hospital-level care. Ocular gonorrhea in adults is a medical urgency; clinicians often use ceftriaxone (e.g., 1 g IM/IV) and saline eye irrigation, with prompt ophthalmology follow-up.
Testing: Smarter Strategies for Better Outcomes
Here’s where many people go wrong: they get a urine test and feel covered. That catches urethral infections in people with penises, but it can miss infections in the throat and rectum. Testing has to match your actual sites of exposure.
How Gonorrhea is Diagnosed
- Nucleic Acid Amplification Tests (NAATs): These are the most sensitive tests and the standard for diagnosis. They can be run on urine, vaginal/cervical swabs, rectal swabs, and throat swabs. Many clinics offer self-collection for throat and rectal swabs with excellent accuracy when instructions are followed.
- Culture: Less sensitive than NAAT for detection, but essential if treatment failure is suspected or to assess antibiotic susceptibility. Culture is also preferred in certain legal or public health contexts, and typically used for ocular infection.
Getting the Right Specimens
Match the Test to the Exposure
- Vaginal Sex: Vaginal/cervical swab (or urine in some settings)
- Insertive Penile Sex: First-catch urine (the first part of the stream)
- Receptive Anal Sex: Rectal swab
- Oral Sex: Throat swab
If you’ve engaged in oral or anal sex without barriers, ask explicitly for throat and/or rectal testing. In my experience, many busy clinics default to urine-only unless someone speaks up or a comprehensive sexual history is taken.
Timing Matters
- Urethral Infections: Often turn positive by NAAT within 3–5 days; throat and rectal can take up to 7–14 days to reach high sensitivity.
- Early Testing: If you test very early after exposure and it’s negative, retesting after the window period is sensible if you remain concerned or symptoms appear.
- Test of Cure: After treatment, a “test of cure” isn’t needed for urogenital or rectal infections unless symptoms persist—except for pharyngeal infections, where a test-of-cure by NAAT at 7–14 days is recommended due to higher risk of persistent infection.
- Retesting: Regardless of test-of-cure, retesting at around 3 months is advised because reinfection rates are high (commonly cited in the 7–12% range within a year).
Who Benefits from Routine Screening
Guidance varies slightly by country, but a practical summary for 2023 looks like this:
- Sexually Active Women Under 25: Annual screening, and beyond 25 if risk factors exist (new partner, multiple partners, partner with an STI).
- Men Who Have Sex with Men (MSM): At least annual screening of all relevant sites (urethra, rectum, throat). Every 3–6 months for those with multiple partners, PrEP users, or those with recent STIs.
- Transgender and Nonbinary People: Screening tailored to anatomy and exposure; don’t let binary checkboxes prevent appropriate throat/rectal testing.
- Pregnancy: Screen early, and again in the third trimester for those at ongoing risk.
- People Living with HIV: At least annual screening at all sites of exposure.
- After Sexual Assault: Testing, prophylaxis, and compassionate follow-up tailored to local protocols.
What to Expect During Treatment
Typical Treatment Experience
Most uncomplicated cases are handled in a single visit:
- Injection of Ceftriaxone: You receive an injection of ceftriaxone—usually in the gluteal muscle or thigh. It stings briefly.
- Chlamydia Co-Infection: If chlamydia hasn’t been ruled out, you’ll also get a prescription, commonly doxycycline for a week (unless pregnant).
- Alternatives Due to Allergies or Access Barriers: If you’re receiving an alternative due to allergies or access barriers, your clinician will explain what to expect.
- Partner Notification: You’ll be asked about partners going back 60 days and how they can be treated—more on that below.
- Abstinence Post-Treatment: You should avoid sex for 7 days after treatment and until any symptoms have resolved. If your partner is treated later, restart the 7-day clock from when the last partner completed treatment.
- Retesting for Reinfection: Plan on retesting at about 3 months to check for reinfection.
Side effects are usually mild—some soreness at the injection site, occasional GI upset if oral meds are involved. If you have severe allergy symptoms (hives, difficulty breathing) after starting treatment, seek urgent care.
When Things Don’t Go as Planned
- Persistent Symptoms: Persistent symptoms after the abstinence period may reflect reinfection, another condition (like nongonococcal urethritis, trichomoniasis, bacterial vaginosis), or, rarely, resistant gonorrhea. Follow up promptly.
- Failed Pharyngeal Treatment: If pharyngeal test-of-cure is still positive at 7–14 days, clinicians will typically re-treat with ceftriaxone and may obtain a culture to assess susceptibility.
- Self-Medicating Risks: Self-medicating with leftover antibiotics or partial courses is a fast track to masking symptoms, not curing infection. It also fuels resistance.
Partner Management: Preventing Ping-Pong Infections
Treating one person without addressing partners is like fixing one rail on a broken train track. Reinfection is common if partners aren’t treated.
Partner Treatment Approach
- Identify Partners: Identify sex partners from the 60 days prior to symptom onset or diagnosis (whichever is earlier). If the last sexual contact was more than 60 days ago, that partner should still be notified and treated.
- Evaluate and Treat Partners: Partners should be evaluated, tested, and presumptively treated without waiting for results.
- Expedited Partner Therapy (EPT): EPT can be a useful tool where legal and appropriate. With EPT, a clinician provides medication or a prescription for your partners without examining them. For gonorrhea, EPT typically uses cefixime 800 mg orally once plus doxycycline for 7 days if chlamydia hasn’t been excluded. It isn’t ideal for suspected pharyngeal infection and doesn’t replace a full exam, but it’s far better than leaving partners untreated.
- Communicate Clearly: Provide straightforward information to partners: what infection, what treatment, and the 7-day abstinence window. Keep it factual and nonjudgmental.
Sample Partner Notification
Sample message partners have found helpful:
- “Hey, I was just treated for gonorrhea. You should get tested and treated, even if you feel fine. It’s easy to handle but can cause problems if untreated. I can send you info from the clinic that saw me.”
If you’re uncomfortable reaching out, many health departments offer confidential partner notification services. They’ll handle the outreach without naming you.
Prevention That Matches Real Life
Perfect is overrated; consistent and realistic beats idealized advice that doesn’t fit your life. Prevention for gonorrhea sits on a few simple pillars, and in clinics we refine them to match someone’s patterns and preferences.
Practical Prevention Tips
- Barriers: Barriers used correctly and consistently reduce transmission. Condoms for vaginal and anal sex are straightforward. For oral sex, condoms (on a penis or sex toy) and dental dams (for oral-vulva or oral-anal) protect the throat and genitals. If condoms break or slip, it’s often because of the wrong size, insufficient lube, or a mismatch between oil-based products (which degrade latex) and latex condoms. Water- or silicone-based lube with latex, oil-based lube with polyurethane/polyisoprene condoms—match them deliberately.
- Screening Cadence: Screen at a cadence that fits your risk. For a monogamous couple with recent negative tests, annual screening may be enough. For someone with multiple partners, group sex, or anonymous encounters, 3–6 month screening at all exposure sites is a better fit.
- Partner Treatment and Abstinence: Treat all partners and pause sex until treatment is complete. Most repeat infections come from untreated partners or new exposures during that 7-day window.
- Doxy-PEP: Consider the broader toolkit if eligible. Doxycycline post-exposure prophylaxis (doxy-PEP) emerged in 2022–2023 studies showing substantial reductions in chlamydia and syphilis and a more modest reduction in gonorrhea among MSM and transgender women at high risk. Programs expanded in some areas through 2023, but it’s not a silver bullet for gonorrhea and comes with stewardship considerations. If you qualify and your clinician recommends it, use it as an add-on, not a replacement for routine screening and condoms during higher-risk acts.
- Vaccines: There isn’t a gonorrhea vaccine yet. Some studies suggest meningococcal B vaccines may offer partial cross-protection, but they aren’t recommended specifically to prevent gonorrhea. If you’re eligible for meningococcal B vaccination for other reasons, that’s a separate conversation with potential side benefits.
Common Mistakes That Lead to Trouble
I’ve seen the same pitfalls derail people over and over. Avoiding these makes a big difference:
- Assuming a Urine Test Covers Everything: If you’ve had oral or anal sex, ask for throat and rectal tests. Many infections hide there.
- Waiting for Symptoms: Silence is common, especially in the throat and rectum. Routine screening catches what your body doesn’t announce.
- Using Leftover Antibiotics: Using antibiotics leftover from another illness or a friend. That’s how resistance spreads and how symptoms get masked without a cure. Gonorrhea requires specific regimens and partner management.
- Resuming Sex Too Soon: The 7-day abstinence window after treatment (and until symptoms resolve) isn’t negotiable if you want to avoid passing it back and forth.
- Not Sharing the News with Partners: It’s awkward, but untreated partners are the top reason people end up in a reinfection loop.
- Relying Solely on Condoms or Testing: Both matter. Condoms cut risk in the moment. Testing catches the misses.
- Ignoring Rectal or Throat Symptoms: Or chalking them up to hemorrhoids or a common sore throat. If the timing fits and you’ve had relevant exposures, ask for site-specific testing.
Real-World Scenarios
Sometimes the best way to see how this plays out is to walk through it.
Scenario 1: The “Just a Sore Throat” After a Hookup
You had receptive oral sex with a new partner last weekend, no condom or dental dam. Three days later, you have a sore throat. You’re not feverish and can swallow fine.
- What Can Be Done: Throat swab NAAT for gonorrhea (and often chlam